As the disease progresses, the correct shape and flexibility of the intervertebral discs are lost: gradual deformation occurs. The distance between the vertebrae decreases, resulting in pinched nerves and pain. Of all parts of the spine, the lumbosacral part is most often susceptible to these pathological changes.
Causes and signs of lumbar osteochondrosis - how does the disease manifest itself?
The disease in question arises from inadequate load distribution on the spine. This is the main reason for the diagnosis of lumbar osteochondrosis. There are many factors that can cause the occurrence and development of this disease.

- Passive lifestyle. This includes people who lead a predominantly sedentary lifestyle. In a sitting position, the corset muscles relax, which increases the load on the lumbar spine.
- Inflammatory phenomena localized in the joints of the spine.
- Dysfunction of the endocrine system, hormonal imbalance.
- Serious infectious diseases of bones and joints (tuberculosis, osteomyelitis).
- Dysfunction of the gastrointestinal tract and heart.
- A lifestyle associated with heavy physical labor (loaders, weightlifters, construction workers).
- Uneven posture, incorrect walking.
- Low density of cartilage tissue (hereditary factor).
- Congenital pathologies related to the structure of the spine/skeletal system. Musculoskeletal system dysfunction.
- Obesity.
- Unbalanced work and rest regime.
- Age. In humans, after the age of 50, the intervertebral discs become less elastic and inactive.
- Chemical poisoning.
- Flat feet. With the correct structure of the foot, the load is absorbed when walking. With flat feet, the intervertebral discs are subjected to maximum stress, which leads to their deformation and destruction.
- Back injury.
The respective symptoms of the disease are divided into three groups. Reflex sign (pain). They have several manifestations:
- Lumbago. Occurs as a result of sudden movements (high jump, running, coughing). This pain is paroxysmal in nature (lumbago). During this attack, the patient leans his upper body forward and remains in this position for a certain period of time: attempts to sit up cause a new wave of pain. Lumbago occurs due to pinched nerve roots.
- Lumbodynia. The pain that occurs in the lumbar region is of an increasing nature. Initially, the patient feels some discomfort, which can develop into severe, regular pain. The cause of lumbodynia can be a sedentary lifestyle and excessive physical activity. Lumbodynia can develop against the background of lumbago.
- Sciatica. Pain sensations spread along the sciatic nerve. The main location is the lower extremities. This phenomenon occurs when the nerve roots of the spinal cord become pinched. When motor fibers are involved in the destructive process, the patient experiences muscle spasms and muscle weakness. Ignoring these symptoms can lead to muscle loss in the future.

Radicular syndrome. Characterized by the following manifestations:
- the skin of the legs regularly loses sensitivity;
- the patient complains of stabbing pain in the lumbar region;
- There are disturbances in the sweating system.
Radicular-vascular signs. They occur against the background of compression of blood vessels. The following complaints are noted by the patient:
- Heat/cold in lower extremities;
- slight tingling/increasing pain in feet;
- Swelling (when veins are compressed).
Lack of appropriate treatment can cause a spinal stroke, which can lead to partial/complete paralysis of the lower extremities and serious dysfunction of the pelvic organs. Lumbar osteochondrosis has a negative effect on the structure of the vertebrae: over time they can become displaced. This violation can provoke a number of negative phenomena.
- Dysfunction of the internal organs and the genitourinary system.
- Frequent fatigue.
- Weakness.
- Irritability.
Symptoms of lumbosacral osteochondrosis depending on the degree - how is the disease diagnosed?
Based on the amount and strength of manifestation of clinical symptoms, the disease in question is divided into several degrees. The first degree is initial, the second degree is mild and the third is severe.
Lumbar osteochondrosis of the 1st degree.
Characterized by main symptoms:
- Lumbago (lumbago), which occurs due to a tear in the disc capsule (intervertebral vertebra).
- swelling of the tissue.
- Muscle cramp.
- Regular pain.
With grade 1 lumbar osteochondrosis, the patient may experience additional symptoms caused by compression of blood vessels and nerve roots.
- Mimicking dysfunction of the kidneys and gastrointestinal tract.
- Periodic abdominal pain that occurs against the background of a spasm of the abdominal muscles.
Lumbar osteochondrosis of the 2nd degree.
This degree of lumbar osteochondrosis is also characterized by the following manifestations:
- Regular pain (lumbodynia). The location of the pain, which can vary in severity, is the lower back.
- Non-standard mobility in the joints of the spine. A tight bandage on the lower back can briefly improve the patient's general condition and relieve pain.
- Malfunctions (not always) of internal organs. In some cases, a patient with lumbar osteochondrosis may experience bronchial asthma and dysfunction of the biliary/urinary tract.
- Pain in the lower extremities going towards the sciatic nerve.
Lumbar osteochondrosis of the 3rd degree.
This level of disease requires surgical treatment, otherwise paralysis and death may occur. The 3rd degree of lumbar osteochondrosis has its peculiarities.
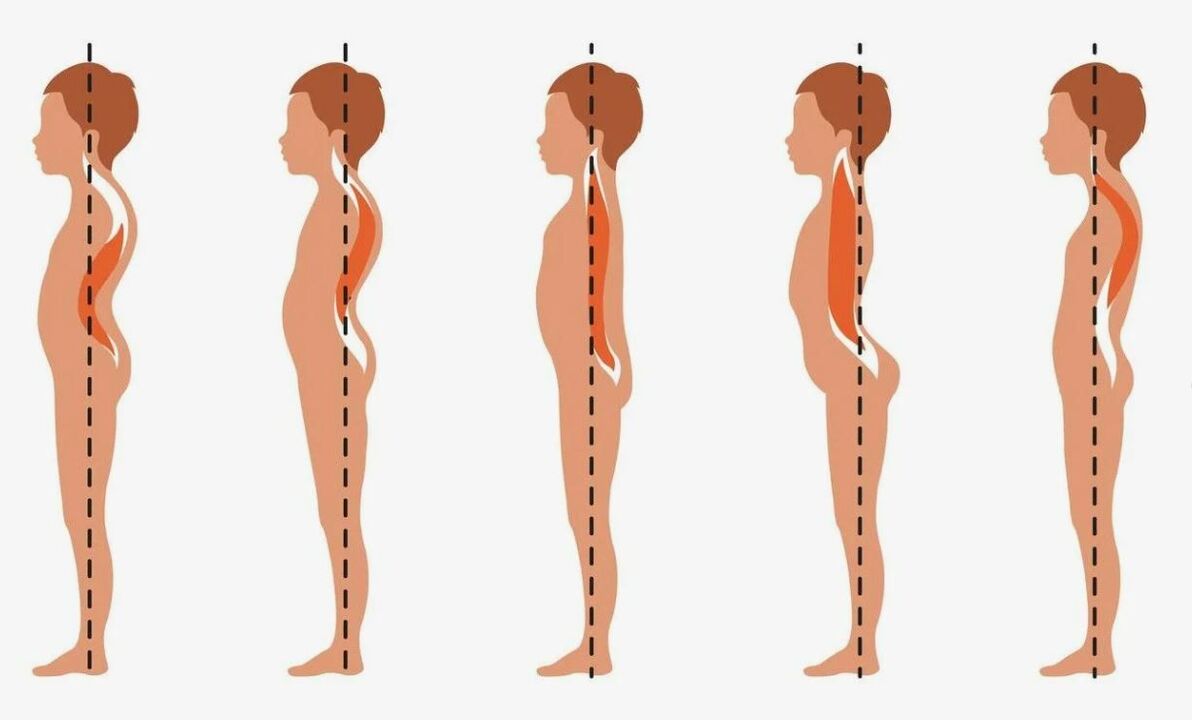
- Spinal deformities: curvature to the right/left (scoliosis); Forward arching (lordosis), protrusion of the lumbar spine (kyphosis).
- Constant, severe, acute pain that becomes noticeable even with the slightest physical activity (changing positions, coughing, sneezing).
- Swelling of muscle tissue and ligaments.
- Periodic/regular loss of sensation in the lower part of the body (lower back, legs, feet).
- Disorders of the urogenital system.
Treatment methods for lumbar osteochondrosis
The choice of treatment tactics for a given disease depends on the degree of osteochondrosis, the presence of additional diseases, the general condition of the patient and other factors that are necessarily taken into account by the attending physician.
There are two important points that any doctor can be guided by when prescribing treatment.
- To eliminate osteochondrosis of the lumbar spine, an integrated approach is required.
- Treatment measures (intensity, duration) are determined by the degree of neglect of the pathology in question.
Drug treatment of lumbosacral osteochondrosis – effective drugs
Every year scientists develop new drugs that help relieve the symptoms of lumbar osteochondrosis. The medication list below does not represent a standard; it can change. However, today doctors often use certain drugs to combat the manifestations of this disease.

- Chondroprotectors. They stop the destructive processes in the cartilage tissue of the spine that occur in the initial stages of the disease.
- Anti-inflammatory (non-steroidal) drugs. Used to treat lumbosacral osteochondrosis of the 2nd degree. This group of drugs can be used in the form of injections (intramuscularly), tablets, ointments, rectal suppositories, capsules and solutions. In case of exacerbation of the disease, the patient may be prescribed injections (16 mg/day).
- Muscle relaxants. Help eliminate discomfort caused by increased muscle tone.
- Vasodilators. Helps to improve blood circulation, prevent stagnation and minimize the risk of infection in the body.
- Local anesthetics. If the pain is severe and persistent, the anesthesiologist will perform a block. A solution is injected into the painful area using a special needle. The pain goes away immediately and does not bother you for several weeks. Such a blockage should only be used in extreme cases: it has many negative consequences.
- Vitamin and mineral complexes. Often prescribed to older patients to increase the strength of tendons and ligaments.
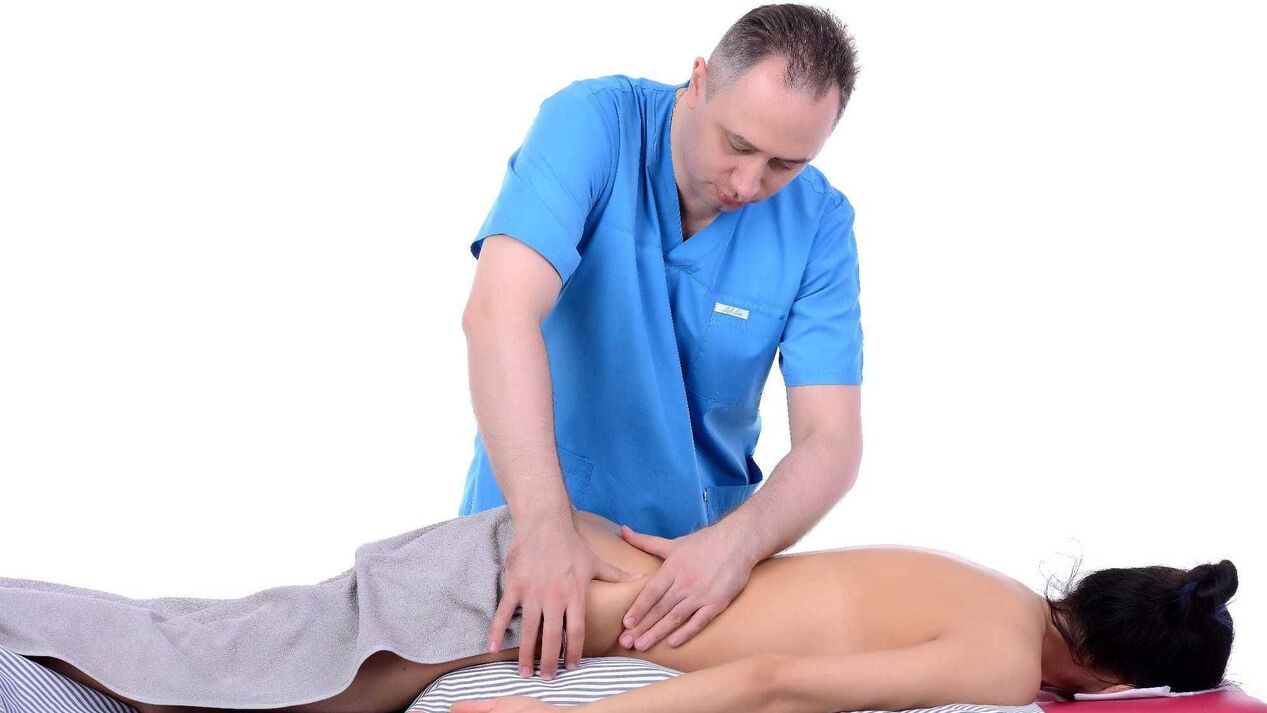
Massage for lumbar osteochondrosis of the lumbosacral region
This method of treatment will be useful in the subacute stage of the disease in question. Through massage it is possible to eliminate pain, eliminate muscle tension and hardness.

The massage should be carried out on a healthy (unaffected! ) area. During the procedure, the patient lies on his stomach on a flat, hard bed. Place a pillow/cushion under your stomach. It is also important to ensure that the patient's legs are elevated (45 degrees). The forehead should rest on a hard surface.
For massage, it is better to use special products (oils, creams, lotions) with warming properties or conduct the session immediately after thermal procedures (bath, sauna). Nowadays there are many massage techniques. Let's highlight the main ones:
- Stroke. There are several types of strokes: hook-shaped, transverse flat, fan-shaped, ending with symmetrical strokes in the area of the sternum muscles.
- To squeeze. Performed in combination with stroking. This massage technique provides muscle stretching.
- Knead.
- Tremble.
- Trituration. Often used to improve the function of tendons, ligaments and joints.
- Point hit. Not every masseur is able to carry out the procedure using the acupressure technique.
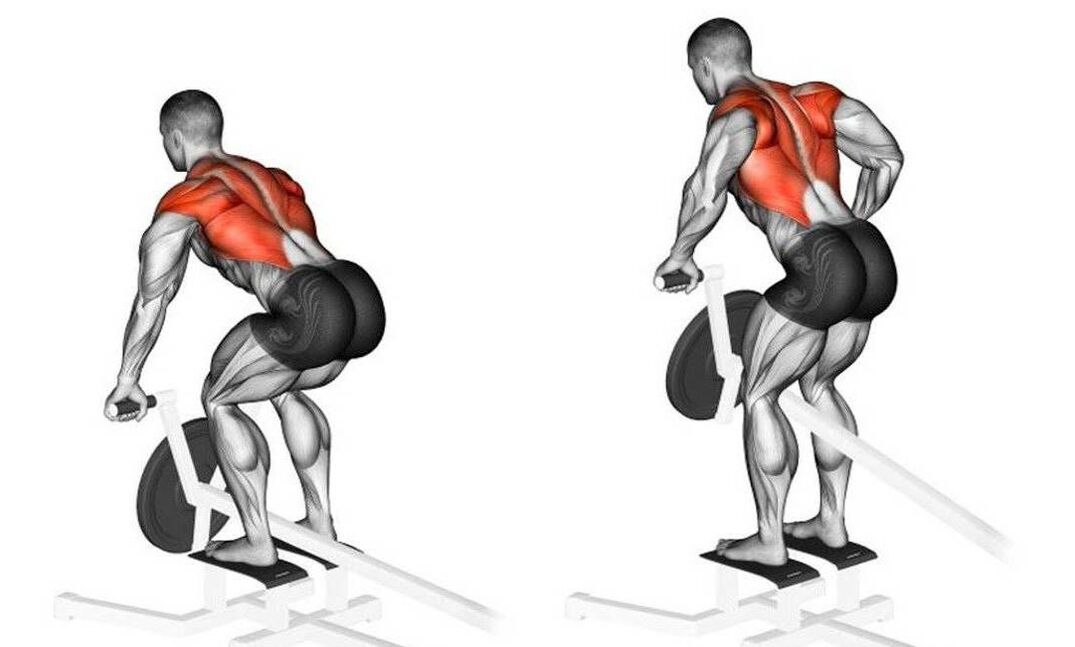
Therapeutic gymnastics or exercise therapy for lumbar osteochondrosis - a set of exercises for the lumbosacral spine in the video.
The entire complex of physical exercises for diagnosing lumbar osteochondrosis is designed to help increase the mobility of the lumbar spine.
Therapeutic gymnastics is not effective if the exercises are performed occasionally. The main principle of exercise therapy is regularity. Constantly performing certain exercises helps to eliminate destructive processes in the intervertebral joints. It is forbidden to carry out exercise therapy for acute pain. If the pain is severe, doctors recommend bed rest and wearing special corsets. When the pain subsides, you can try therapeutic exercises.
Physiotherapy for lumbar osteochondrosis
This method of conservative treatment is one of the most effective. However, to achieve the desired result, a lot of time must be spent. Using multiple types of physical therapy at the same time helps speed recovery. This method of treatment has many contraindications that cannot be ignored. Physiotherapy is often prescribed to children, pregnant women, nursing mothers and elderly patients.
The use of physiotherapy is prohibited in the following cases:
- Cancer;
- acute stages of osteochondrosis;
- serious dysfunction of the central nervous system;
- Injury to the area where physical therapy should be performed.
Nowadays, a number of physiotherapeutic procedures have become widespread in the treatment of lumbar osteochondrosis.
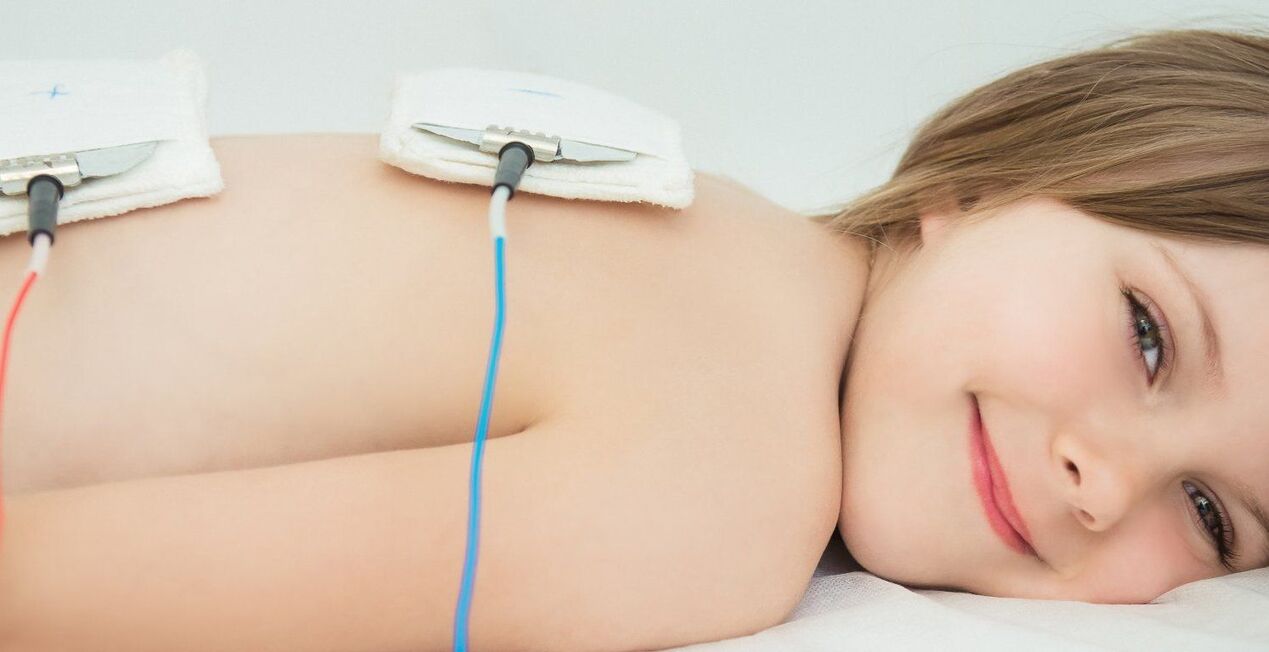
- UV radiation. The pathological area is exposed to heat, which helps to improve blood supply, eliminate spasms and relieve pain.
- Magnetic field therapy, electrophoresis. When using the method, the painful area of the spine is exposed to a magnetic/electric field. Due to this effect, it is possible to regulate the body's metabolic processes, eliminate inflammatory phenomena (completely/partially) and accelerate recovery.
- Laser therapy. The condition of the affected spinal roots is significantly improved by the influence of helium-neon emitters on them.
- Balneotherapy. The main ingredient used to carry out each physical treatment is healing mud and mineral water.
- Detensor therapy (mechanical stretching of the spine). Relevant for severe back pain.
Folk remedies for lumbar osteochondrosis
This treatment method uses ointments, rubs and compresses with medicinal plants. Such funds help reduce inflammation and eliminate pain. It is advisable to use folk remedies with caution in the treatment of lumbar osteochondrosis: an allergic reaction may occur/develop.
In the fight against the disease, rubs and compresses are often used:
- Red pepper tincture: for rubbing painful areas in the lower back. To prepare the drug you need to mix 1 tbsp. Vodka (diluted medical alcohol), 20-25 gr. dry ground red pepper. It is necessary to let these ingredients brew (stir occasionally) for 5-7 days.
- Camphor and mustard: for daily rubbing before bed. To prepare the product, mix mustard powder (50 g), camphor alcohol (50 ml), medical alcohol (90-100 ml) and whipped egg whites (3 pieces). After mixing thoroughly, a liquid ointment should form.
- Honey and aloe: for compresses on the lower back (twice a day). To prepare this product you will need honey (100 ml), diluted medical alcohol (150 ml) and aloe juice (50 ml). Before using, this mixture should rest for 10-12 hours.
- Horseradish root and alcohol: for rubbing into the affected area of the back. To prepare this product, mix horseradish root juice and medicinal alcohol in equal proportions. After rubbing, wrap the treated area.
- Garlic juice and pork fat (1: 2): for rubbing into painful areas of the lower back.
- Cabbage leaf peeled from thick veins: for compresses. Before application, the cabbage leaf should be immersed in hot (not more than 60 ° C) water. You can attach the sheet to the lower back with a bandage/gauze. After changing the leaf color, the process can be repeated.

Prevention of lumbar osteochondrosis
A whole range of measures are required to prevent the respective disease.
Right nutrition. The diet should be balanced and low in calories. It is not recommended to eat meals more than 6 times a day. Certain foods should predominate in your daily diet.
- Fish (sea).
- Vegetable fats (olive oil, linseed oil).
- Dairy products with a minimum content of colorings and sugar.
- Dishes containing gelatin (aspic, jelly).
- Animal cartilage (can be used to prepare first courses).
- Fresh fruits, vegetables.
- Green.
- Mineral water.
Taking vitamin and mineral complexes (1-2 times a year) makes sense.
Active lifestyle
- Bathe.
- Daily walks.
- Gymnastic exercises (also suitable for pregnant women).
Performing simple physical exercises (15-20 minutes per day) to strengthen the back muscles.
Lumbar osteochondrosis can progress from the acute to the chronic stage, which means annual expenses for massages, pain-relieving injections and warming ointments. If you do not treat all this, the consequences can be very sad, up to paralysis or death!



























